Blog | Specialized Care
Intracranial Atherosclerotic Disease: A Slow But Sure Path to Brain Destitution
published: 5/21/2025
viewedby 28117 visitors
Introduction
Intracranial atherosclerotic disease (ICAD) is an accumulation of plaque (fatty deposits) within the wall of the brain’s arteries. Left untreated, this buildup of sticky substance will slowly but surely either (i) cause arterial narrowing, which eventually promotes arterial occlusion, or (ii) rupture, which induces arterial embolization. Both lead to ischemic stroke, the leading cause of death and disability worldwide.
1. Epidemiology
Recent studies reported that ICAD was identified as the major cause of ischemic stroke among Asian, Hispanic, and African-American populations (30-70%). This peculiarity is believed to be caused by variations in diet, lifestyle, genetic susceptibility, environment, and certain risk factors, such as:
- Older age
- Hypertension/elevated blood pressure
- Hyperlipidemia/elevated cholesterol level
- Diabetes mellitus
- Smoking
2. Symptoms & Signs
ICAD may not show symptoms or signs if blood delivery to the brain is still adequate. However, when arterial narrowing, occlusion, or embolization occur, ICAD may lead to transient ischemic attack (a reversible condition of brain ischemia) or ischemic stroke and produce its characteristic symptoms or signs:
- Facial droop
- Arm/leg weakness
- Slurred speech
- Double vision
- Dizziness/vertigo
- Loss of consciousness
Without proper and timely management, ischemic stroke may result in irreversible disability, devastating complications, and death.
3. How ICAD Can Produce Stroke?
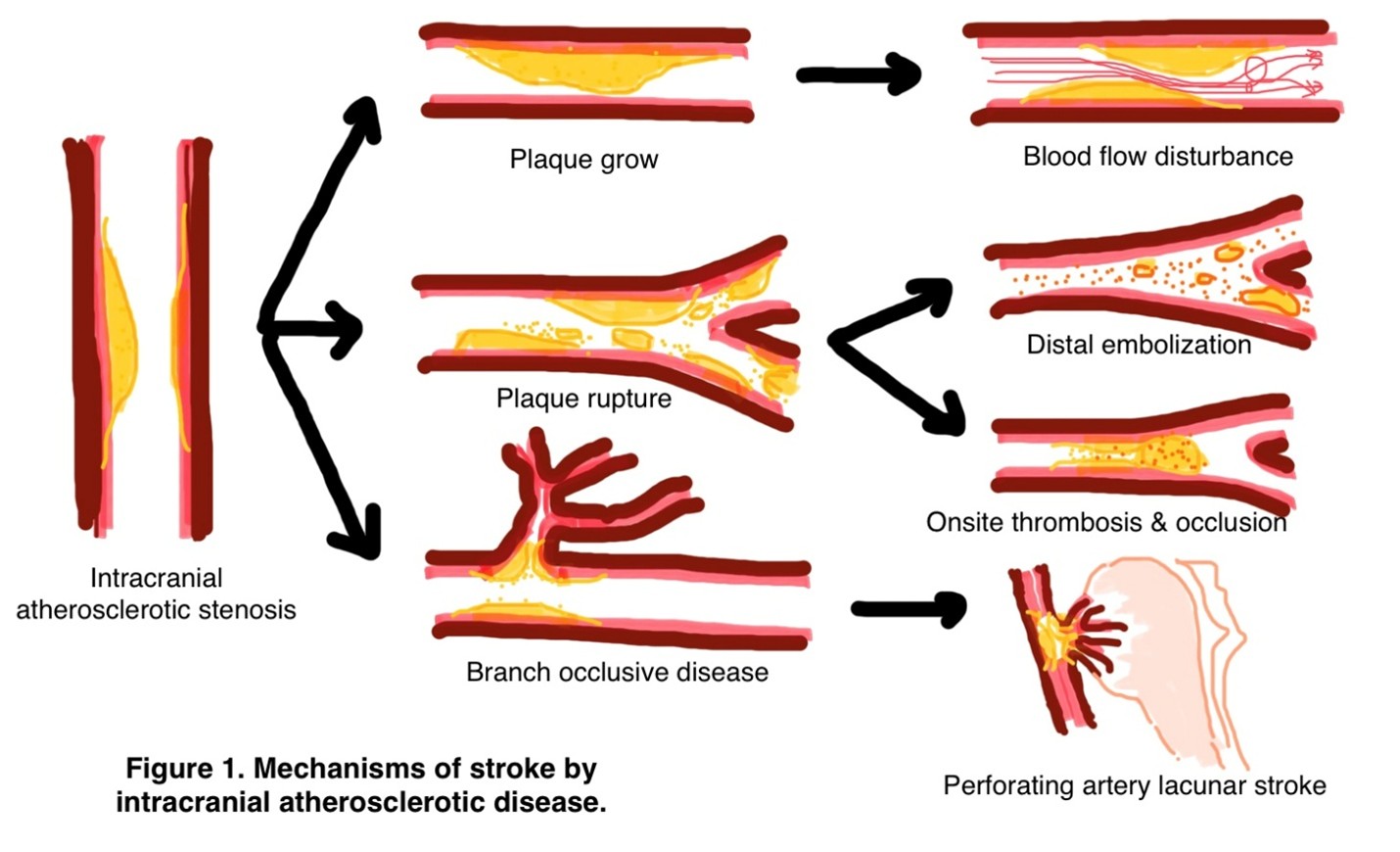
ICAD may produce stroke through these mechanisms (see Figure 1):
- Artery-to-artery embolization: blockage due to floating ruptured plaque emboli
- Perforator disease: occlusion due to small-sized end/distal artery atherosclerosis
- Hypoperfusion: blood delivery impairment in the watershed/border zone areas (unique areas in the brain located between the territories of major brain arteries, where blood supply usually decreases)
4. Diagnosis
Laboratory
Several laboratory remarks may be associated with the presence of ICAD:
- Elevated leucocyte, neutrophils, neutrophil-to-lymphocyte ratio (NLR), and homocysteine
- Elevated lipid ratios:
o Total cholesterol/high-density lipoprotein-cholesterol (TC/HDL-C)
o Low-density lipoprotein-cholesterol/high-density lipoprotein-cholesterol (LDL-C/HDL-C)
o Remnant cholesterol/high-density lipoprotein-cholesterol (RC/HDL-C)
o Non-HDL-C/HDL-C
o Apolipoprotein B (apo B)/HCL-C
o Apo B/apolipoprotein A-1 (apo A-1)
- Elevate interleukin-6 (IL-6) and matrix metalloproteinases (MMPs)
Radiology
Focused radiologic examinations are available to assist in the diagnosis of ICAD:
- Lumen (intravascular cavity)-based:
o Computed tomography angiography (CTA)
o Magnetic resonance angiography (MRA)
o Digital subtraction angiography (DSA)
o Intravascular ultrasound (IVUS)
- Haemodynamic (blood flow/velocity)-based:
o Transcranial Doppler (TCD)
o Perfusion imaging
o Computation fluid dynamics
- Arterial wall-based:
o High-resolution vessel wall MRI (vwMRI)
- Functional studies of plaque composition:
o 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET)
o Optical coherence tomography
Classification
Based on the examinations mentioned above, the degree of the blood vessel narrowing may be categorized into:
- Normal (0-9%)
- Mild (10-29%)
- Moderate (30-69%)
- Severe (70-99%)
- Complete occlusion (100%)
Differential Diagnoses
ICAD may be misdiagnosed with these other conditions that may mimic its presence:
- Moyamoya disease: an isolated chronic vasculopathy (blood vessel disease) of unknown cause, characterized by progressive narrowing of the terminal intracranial portion of the internal carotid artery and circle of Willis
- Vasculitis: rare blood vessel inflammation
- Reversible cerebral vasoconstriction syndrome: reversible narrowing of the brain blood vessels that may be triggered by a pregnancy-related condition (e.g., puerperium, eclampsia), illicit drugs (e.g., cocaine, LSD), as well as licit drugs (even coffee!)
- Arterial dissection: a tear within the wall of brain arteries that creates a false lumen (pocket) within the arterial wall
- Intraluminal thrombus: a blood clot within the arterial cavity that is attached to the arterial wall distally
5. Management
Management can be divided into medical, surgical, and endovascular treatment.
- Medical:
o Antithrombotic therapy: dual antiplatelet therapy (aspirin and clopidogrel)
o Risk factor modification: smoking cessation, application of a healthy diet (particularly Mediterranean diet), and ideal physical activity
o Lipid-lowering treatments: statin/HMG-CoA reductase inhibitors
- Surgical:
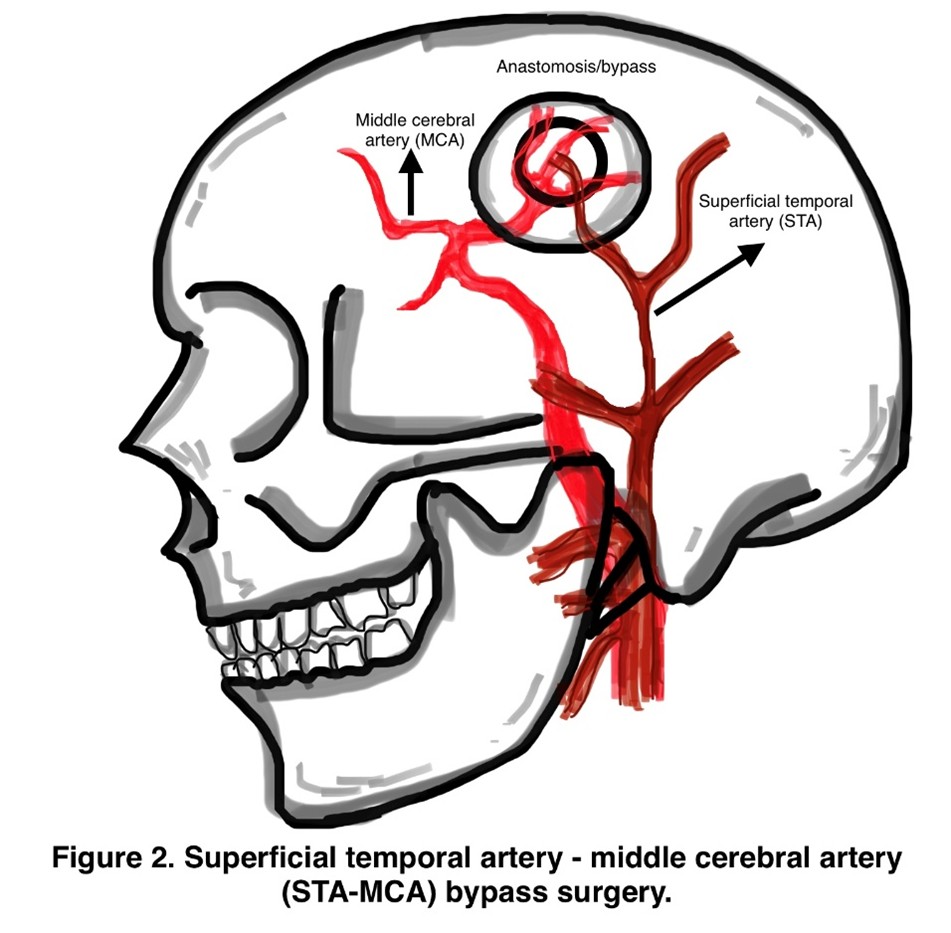
o Bypass surgery: surgery to connect any external carotid artery (ECA) branches to internal carotid artery (ICA) branches (e.g., STA-MCA bypass [Figure 2])
o Encephaloduroarteriosynangiosis (EDAS)
- Endovascular
o Angioplasty and stenting: intravascular procedures to dilate narrow blood vessels. This procedure is currently reserved only for selected patients with recurrent stroke.
6. What to do when you experience/witness others experiencing the symptoms/signs of ICAD?
Please visit the nearest health care facility with the proper resources to manage the ICAD (neurologists and/or neurosurgeons present, 24-hour catheterization lab and operating theaters). Do not waste time. Each second matters.
References
Chen LH, Spagnolo-Allende A, Yang D, Qiao Y, Gutierrez J. Epidemiology, Pathophysiology, and Imaging of Atherosclerotic Intracranial Disease. Stroke. 2024 Feb;55(2):311-323. doi: 10.1161/STROKEAHA.123.043630. Epub 2024 Jan 22. PMID: 38252756; PMCID: PMC10827355.
Flusty B, de Havenon A, Prabhakaran S, Liebeskind DS, Yaghi S. Intracranial Atherosclerosis Treatment: Past, Present, and Future. Stroke. 2020 Mar;51(3):e49-e53. doi: 10.1161/STROKEAHA.119.028528. Epub 2020 Feb 10. PMID: 32078441; PMCID: PMC7041867.
Kim JS, Caplan LR, Wong KS. Intracranial atherosclerosis: pathophysiology, diagnosis, and treatment. In: Frontiers of Neurology and Neuroscience. Basel: Karger; 2016.
Panagiotopoulos E, Stefanou MI, Magoufis G, Safouris A, Kargiotis O, Psychogios K, Vassilopoulou S, Theodorou A, Chondrogianni M, Bakola E, Frantzeskaki F, Sidiropoulou T, Spiliopoulos S, Tsivgoulis G. Prevalence, diagnosis and management of intracranial atherosclerosis in White populations: a narrative review. Neurol Res Pract. 2024 Nov 11;6(1):54. doi: 10.1186/s42466-024-00341-4. PMID: 39523357; PMCID: PMC11552123.
about_author
Dr. Aryandhito Widhi Nugroho, M.D., Ph.D

Neurosurgeon, Bali International Hospital
Dr. Aryandhito Widhi Nugroho, Ph.D., is a highly accomplished neurosurgeon with a robust academic and clinical background. He earned his Neurosurgery degree from Universitas Indonesia in 2020, complemented by a Doctor of Philosophy (Ph.D.) from Shiga University of Medical Science in Japan, completed in 2018. His medical journey began with an M.D. from Universitas Indonesia in 2007, laying the foundation for his expertise in advanced neurosurgical techniques. In addition to his clinical roles, he also serves as an lecturer and researcher at the Faculty of Medicine, Khairun University, North Maluku. Fluent in both English and Indonesian, Dr. Dhito is committed to delivering exceptional patient care while contributing to the development of future medical professionals. His international training and diverse experiences make him a key figure in the field of neurosurgery in Indonesia.