Blog | Specialized Care
Abdominal Aortic Aneurysm: The Silent Threat You Shouldn’t Ignore
published: 5/10/2025
viewedby 198 visitors
Introduction
Most of us know Albert Einstein, but did you know what caused his death? He died from an abdominal aortic aneurysm — a serious condition that often shows no symptoms until it suddenly becomes life-threatening.
Einstein had been diagnosed but chose not to have surgery. When told the aneurysm could rupture, he simply said, “Let it burst.”
This condition is often called a “silent time bomb” because it grows slowly and quietly. By the time you feel any symptoms, it might already be too late.

1. What exactly is an Abdominal Aortic Aneurysm?
An aneurysm is a widening of a blood vessel that bulges out like a balloon and can occur in any blood vessel. If it gets too big, it can burst — and that’s extremely dangerous.
The most common type is an abdominal aortic aneurysm (AAA). This happens when the largest blood vessel (the aorta) in your belly becomes enlarged and weakened.
Doctors say it’s an aneurysm if the aorta is:
•Over 30 mm wide in men
•Over 27 mm wide in women
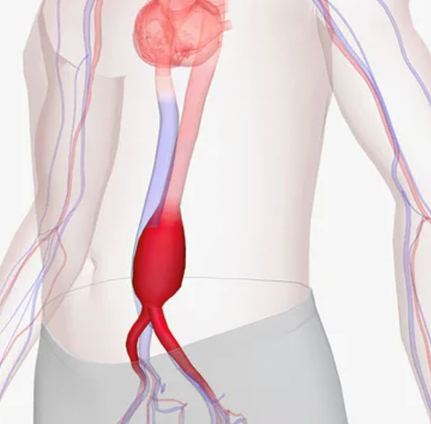
Over time, this bulge can get bigger and eventually burst, causing internal bleeding. A rupture like that can be deadly if not treated immediately.
2. What causes it?
As we age, our blood vessels can become weaker and less flexible. If blood pressure is high or there’s a lot of stress on the vessel walls, they may stretch too much and form an aneurysm. Smoking, genetics, and certain medical conditions can all play a role.
3. Who is at risk?
You’re more likely to develop an AAA if:
•You’re 65 or older
•You smoke (past or present)
•You have high blood pressure
•You have high cholesterol
•You’ve had heart or artery problems
•A close relative has had an AAA
•You have a connective tissue disorder (like Marfan or Ehlers-Danlos)
•You’re male (but women are more likely to have a rupture if they do develop an AAA)
4. How do you know if you have one?
The truth is, you probably won’t feel anything — that’s why it’s dangerous.
Most AAAs are found by accident during exams or imaging for other reasons. The best way to find out is through a simple, non-invasive ultrasound test.
If a doctor finds an aneurysm, they’ll usually measure it and monitor it regularly and a CT angiography scan may follow.
5. How is it treated?
Most AAAs grow slowly and may not need immediate surgery. If it's small, doctors will just monitor it regularly and recommend lifestyle changes like quitting smoking and managing blood pressure.
However, it’s time for treatment if the aneurysm:
•Grows larger than 5.5 cm in men, or
•Larger than 5 cm in women, or
•Grows more than 1 cm per year,
There are two main types of procedures:
•Open surgery – the damaged part of the aorta is replaced with a graft.
•EVAR (Endovascular Aneurysm Repair) – a less invasive option where a stent graft is inserted through blood vessels to strengthen the weak area. This is gentler on the body and suitable for high-risk patients.
6. Don´t wait until it´s too late
Because an abdominal aortic aneurysm usually doesn’t cause symptoms, many people have it without knowing. That’s why screening is so important, especially for those over 65. If you’re 65 or older, especially if you’ve ever smoked, talk to your doctor about getting screened for an abdominal aortic aneurysm. A quick ultrasound could save your life.
about_author
Dr. Rio Marnoto

Consultant, Bali International Hospital
Dr. med. Rio Marnoto is a distinguished consultant in Vascular Surgery, currently serving at the München Klinik Neuperlach in Munich, Germany. Dr. Marnoto's extensive training and expertise are grounded in a solid academic and practical foundation established in some of Germany's most medical institutions. His medical journey began with a rigorous surgical residency at the Department of Vascular und Endovascular Surgery at Universitätsklinikum Augsburg, spanning from 2012 to 2019. During this period, Dr. Marnoto mastered a variety of complex vascular and endovascular procedures, setting a high standard of care in the treatment of vascular diseases. Following his residency, Dr. Marnoto took on the role of an Attending Vascular Surgeon at the same institution in Augsburg from 2019 to 2021, where he further refined his surgical skills. In 2021, he was appointed Head of Phlebology, where he led initiatives to improve treatments for venous diseases, enhancing patient outcomes through innovative surgical techniques